Occupational Cancer Trends Among Canadian Firefighters: Implications for Health, Safety, and Governance
Executive Summary Report
Introduction
This article is based on a peer-reviewed publication in the journal Injury Epidemiology, published online by Springer Nature on December 17, 2025. The study provides the most comprehensive national analysis to date of firefighter injury and fatality claims in Canada between 2007 and 2021.
Canadian firefighters know the risks of the job extend far beyond the fireground. Recent national data on injury and fatality claims show that cancer, traumatic injuries, and mental health disorders are reshaping the health profile of our profession. Between 2007 and 2021, more than 29,000 accepted claims were reported across Canada, underscoring firefighting as one of the most hazardous occupations in the country.
The Reality of Injury and Fatality in Canada’s Fire Service
Between 2007 and 2021, Canadian firefighters submitted 1,509 fatality claims and 27,990 time-loss injury claims.
Fatalities were dominated by cancer, accounting for 84.6% of firefighter deaths, with a fatality rate of nearly 994 per 100,000 firefighters per year. Cardiovascular disease (CVD) and traumatic incidents followed as secondary contributors.
Time-loss injuries were overwhelmingly traumatic in nature, representing 80.6% of claims at a rate of 17,859 per 100,000 firefighters per year. Musculoskeletal strains, sprains, and overexertion injuries were particularly prevalent.
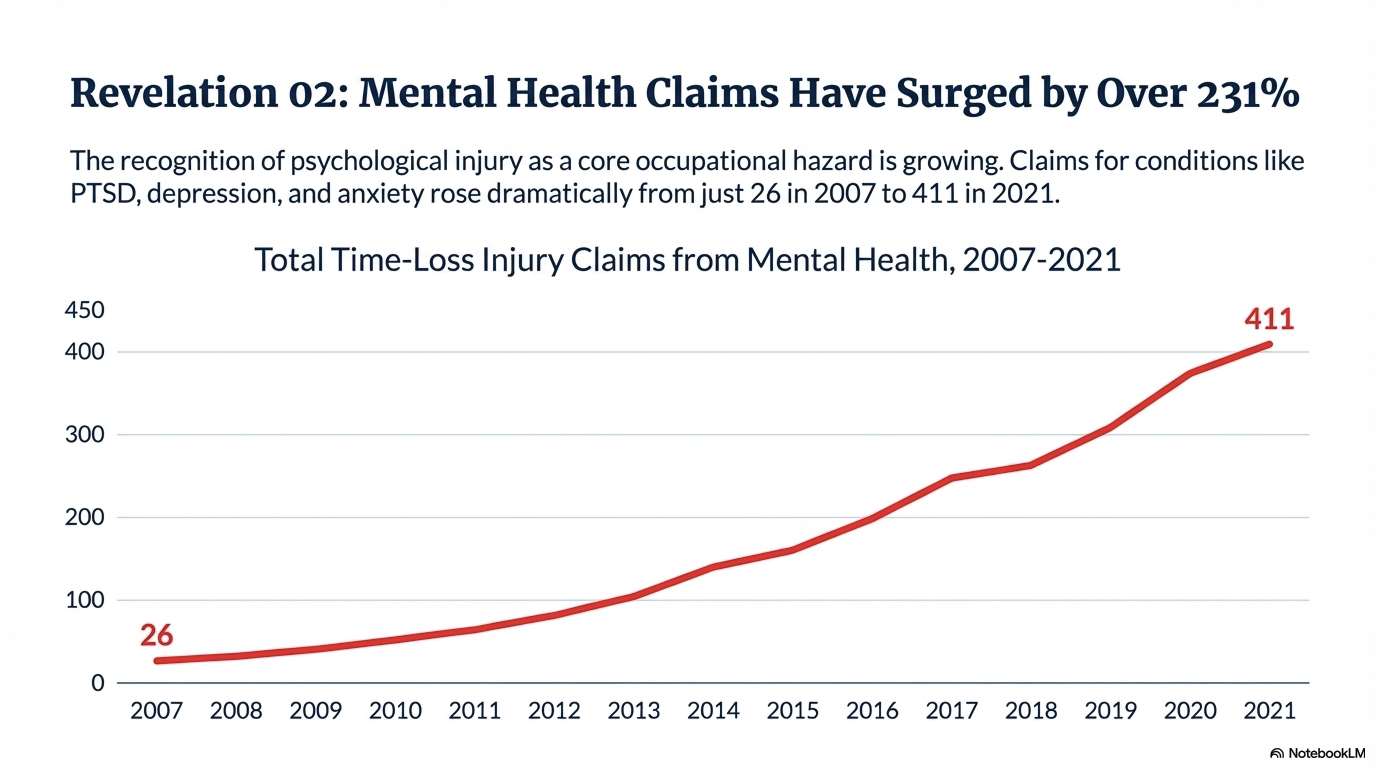
Mental health claims rose sharply, increasing by 231% over the study period, reflecting the growing toll of post-traumatic stress disorder (PTSD), depression, and burnout.
These findings confirm what many in the fire service already know: the health reality of firefighting is shifting from acute trauma toward chronic disease and psychological stress.
Demographic and Provincial Trends
Fatality claims were most common among firefighters aged 65 and over, reflecting the long-term latency of cancer and cardiovascular disease. Time-loss injuries peaked among those aged 30–49, the prime working years of the profession.
Men accounted for 99.4% of fatality claims and 92.2% of injury claims, reflecting the male-dominated composition of Canada’s fire service.
Ontario reported the highest incidence, with 47.3% of fatalities and 30.7% of injuries, followed by Quebec, British Columbia, and Alberta. These provinces represent the largest firefighter populations and the most complex fire environments, from dense urban centres to expansive wildland interfaces.
Cancer: The Leading Cause of Firefighter Fatalities
Cancer continues to stand out as the most significant occupational health threat for Canadian firefighters. More than four out of five fatality claims between 2007 and 2021 were cancer-related. This reflects decades of exposure to toxic combustion products, flame retardants, and hazardous chemicals embedded in firefighting gear.
The latency of cancer means that many firefighters only experience its impact late in their careers, with the majority of fatality claims occurring among those aged 65 and older. Yet the data also show that 14 firefighters aged 25–29 died from occupational causes during the study period, representing nearly 1% of all fatalities. This finding underscores that cancer and other occupational diseases are not confined to retirement years — they can affect firefighters much earlier in their careers.
What makes this picture even more concerning is evidence from prior research showing that only 14% of firefighters had undergone cancer screening in the three years before the study cohort was assessed. This statistic underscores a critical gap: while firefighters face elevated exposure risks, they are not consistently accessing preventive health monitoring. The result is late detection, poorer outcomes, and higher fatality rates.
For the firefighting community, the message is clear. Cancer prevention is not only about reducing exposure on the fireground through decontamination protocols and safer gear — it is also about embedding routine screening and health surveillance from the earliest stages of a firefighter’s career. Screening should be treated with the same seriousness as fitness testing or PPE checks. Administration and unions have a role to play in advocating for funded, accessible screening programs, while departments can lead education campaigns that normalize early detection.
By combining exposure reduction with proactive health monitoring, the fire service can begin to shift the trajectory of cancer outcomes. This is not simply a medical issue — it is a governance and operational priority that directly affects firefighter longevity, workforce sustainability, and community trust.
Cardiovascular Disease: A Silent Killer
Sudden cardiac arrest remains a leading cause of firefighter fatalities during emergency response in North America. Canadian data mirror this global trend.
Firefighters are significantly more likely to die from CVD during emergency response compared to non-emergency duties. Risk factors include obesity, hypertension, diabetes, and musculoskeletal disorders—all prevalent within the firefighter population.
Operational planning must therefore integrate cardiovascular screening, fitness programs, and fatigue management policies into fire service governance. Addressing cardiovascular risk is as much about organizational culture as it is about individual health.
Mental Health: The Rising Tide
The sharp increase in mental health claims—rising from 26 in 2007 to 411 in 2021—signals a cultural and operational shift. PTSD, depression, anxiety, and substance abuse are increasingly recognized as occupational hazards.
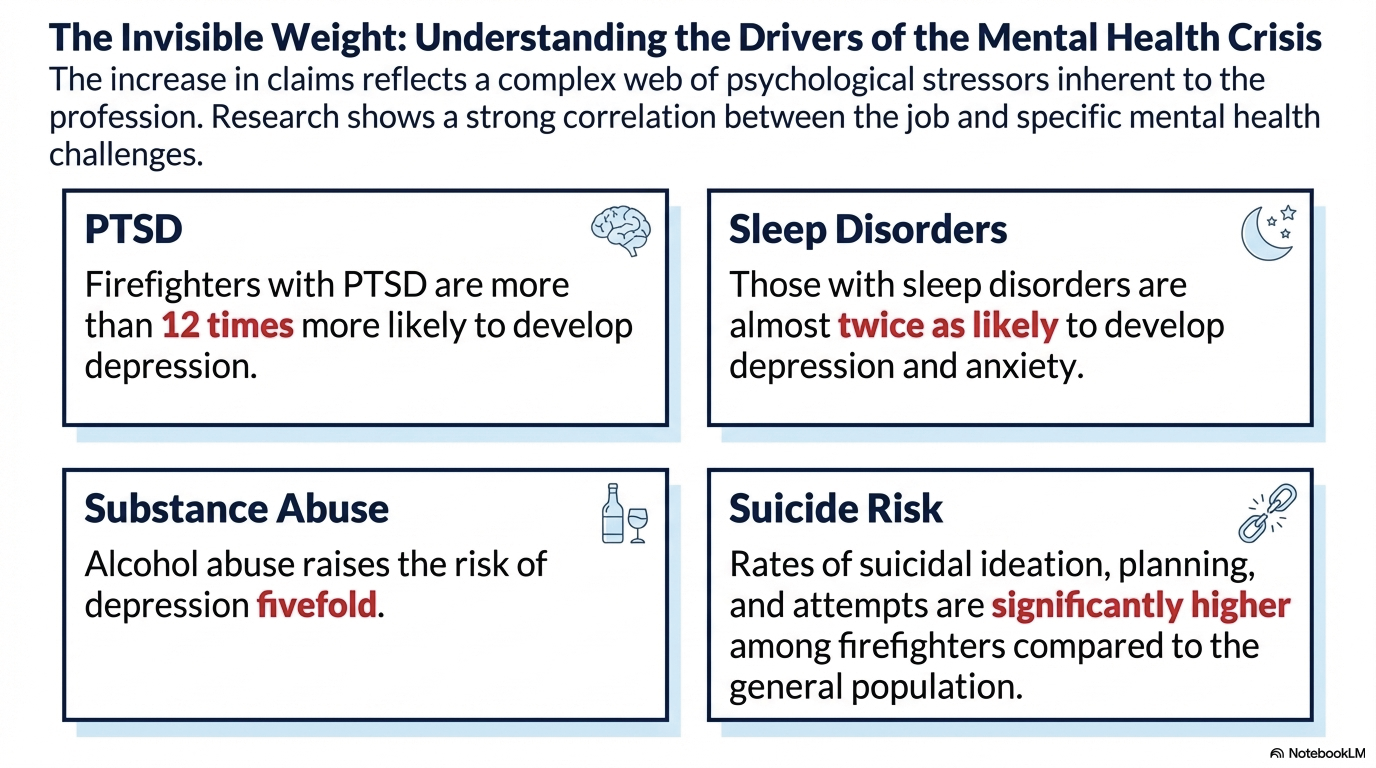
Firefighters with sleep disorders are almost twice as likely to develop depression and anxiety. PTSD increases the odds of depression more than twelvefold, while alcohol abuse raises risk fivefold. Rates of suicidal ideation and attempts are significantly higher among firefighters compared to the general population.
For the firefighting community, this trend demands comprehensive mental health strategies, including peer support programs, confidential counselling, and proactive monitoring. The stigma surrounding psychological injury must be dismantled to ensure firefighters receive timely care.
Operational and Governance Implications
The epidemiological findings carry direct implications for Canadian fire governance and administrative decision-making.
Cancer and cardiovascular screening protocols, integrated mental health assessments, musculoskeletal injury prevention, enhanced decontamination protocols, and harmonized compensation processes are all critical steps.
Building Sustainable Firefighter Health Programs
The findings from 2007–2021 highlight the urgent need for sustainable, evidence-based health programs that empower firefighters and reassure administration of long-term governance accountability.
Community empowerment, national standards, and administrative engagement are all critical. By reframing firefighter health as a governance priority, administration can ensure that occupational risks are mitigated, workforce sustainability is preserved, and public trust in fire services is strengthened.
Strategic Approaches for Firefighter Health and Safety
For the firefighting community, advancing towards a healthier future demands a commitment to evidence-based governance, the implementation of proactive health surveillance, and the establishment of sustainable safety programs. These strategies should be grounded in ongoing research and data to ensure that interventions remain relevant and effective over time.
Investing in firefighter health is not only a matter of supporting those who serve but also a strategic decision for the long-term resilience of Canadian fire services. By prioritizing these investments today, Canada stands to cultivate a fire service that is robust, adaptable, and fully capable of safeguarding communities in the years ahead.
Furthermore, those who finance and support these programs will ultimately realize substantial benefits. Reduced costs associated with preventable injuries, illnesses, and other health-related setbacks will result in a more sustainable allocation of resources, ensuring that both operational efficiency and fiscal responsibility are achieved.
Conclusion
The evidence is clear: Canadian firefighters face a dual challenge of acute traumatic injury and chronic disease, with cancer, cardiovascular illness, and mental health disorders leading the charge. These risks translate into thousands of claims, hundreds of fatalities, and immeasurable impacts on families, communities, and fire services.
Len Garis is Fire Chief (ret) for the city of Surrey, B.C., Research Associate – University of the Fraser Valley, associate scientist emeritus with the B.C. Injury Research and Prevention Unit. Contact him at lwgaris@outlook.com.
Todd Schierling is the president of the BC Professional Firefighters Association, a captain with the Surrey Fire Services and an IAFF 6th District field service representative. Contact him at president@bcpffa.org.
Reference
Al-Hajj, S., Thomas, L., Garis, L., El-Asmar, K., El-Hajj, F., & Pike, I. (2025). Occupational injury among firefighters in Canada: a trends analysis of fatality and time-loss injury claims (2007–2021). Injury Epidemiology, 12:85. Published online December 17, 2025. Springer Nature.
Review the full article here https://doi.org/10.1186/s40621-025-00639-0